Sight-Saving Advances in Diabetic Eye Disease
Written By: Reena Mukamal on October 16, 2020 for the American Academy of Ophthalmology.
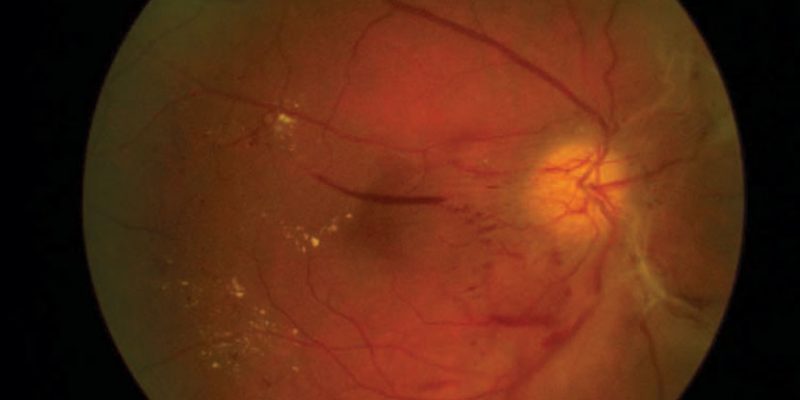
Nearly 10% of Americans have diabetes — a figure that’s expected to double by 2050. As diabetes becomes more common, an unprecedented number of patients will develop a potentially blinding eye complication called diabetic retinopathy.
Fortunately, doctors are developing new tools to detect and treat this condition.
“These new technologies and insights could help more patients preserve their sight and keep doing the things they love, with fewer interruptions to their daily lives,” says says ophthalmologist and Academy member Atma Vemulakonda, MD.
Here’s a rundown of medical advances on the horizon for people with diabetes.
Artificial intelligence can detect eye damage from diabetes
It’s important to spot signs of diabetic retinopathy as early as possible to prevent vision loss. But not every patient with diabetes has access to an ophthalmologist or optometrist. As the number of people with diabetes grows, the shortage of eye care specialists will become a serious problem.
Artificial intelligence (AI) systems can meet this growing demand by analyzing eye photographs for signs of diabetic retinopathy. These AI systems are trained to spot the difference between images of healthy and unhealthy eyes. The U.S. Food and Drug Administration has approved two AI devices for detecting diabetic retinopahy: the IDx-DR and the EyeArt AI Screening System. These systems are designed for use during a patient’s regular office exam. A camera takes pictures of both eyes. These images are then examined and results are available within minutes.
“AI diagnostics represent one of the biggest potential game-changers for diabetic retinopathy,” Dr. Vemulakonda says. “They can help us cast a much wider net and catch more patients who need treatment in a more efficient way. Expansion and automation of DR screening is critical to get in front of the tidal wave of diabetes diagnoses ahead of us.”
New treatments may eliminate need for ongoing eye injections
Today, many patients with diabetic retinopathy take anti-VEGF medications to stabilize or improve their vision. These drugs — including Avastin, Eylea and Lucentis — stave off swelling and broken blood vessels in the retina, which can result from high blood sugar. They also prevent growth of abnormal blood vessels. But there’s a drawback: The drugs must be injected into the eye on a regular basis, as often as 12 times per year.
Two new therapies may provide an alternative to ongoing eye injections.
Gene therapy
Scientists are developing a gene therapy that helps the eye make its own anti-VEGF medicine, with the goal of providing a ‘one and done’ treatment. It works by inserting a harmless virus carrying the anti-VEGF gene into a patient’s own DNA. Two different approaches are being tested. The first treatment, RGX-314, requires a single injection under the retina. This is performed in an operating room. The second therapy, ADVM-022, can be injected into the eye in the doctor’s office. Both methods are in phase 2 clinical trials. It may be two or more years before they become available to the public.
Port delivery system
The port delivery system (PDS) is a tiny refillable device that stores anti-VEGF medicine. Surgery is needed to implant the port, which is about the size of a grain of rice, into the wall of the eye. The system continuously releases anti-VEGF medicine into the eye and can be refilled during an office visit. Some patients may not need a repeat treatment for as long as nine months. The PDS is currently in phase 3 clinical trials and may be on the market within a couple of years.